Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology / etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Cite this page: Saliba E, Brem CE. Lichen sclerosus. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorlichensclerosus.html. Accessed May 11th, 2024.
Definition / general
- Immune mediated chronic mucocutaneous disorder involving both genital and extragenital skin
Essential features
- Sclerotic shiny, ivory colored papules and plaques
- Most commonly female or male genitalia, less often extragenital skin
- Lichenoid interface dermatitis with epidermal atrophy and progressive sclerosis / homogenization of papillary dermal collagen fibers
Terminology
- Current preferred nomenclature of lichen sclerosus (LS) initially proposed in 1975 (J Cutan Pathol 1976;3:159)
- Other names
- Lichen sclerosus et atrophicus
- White spot disease
- Csillag disease
- Lichen albus
- Leukoplakia
- Kraurosis vulvae
- Balanitis xerotic obliterans
ICD coding
Epidemiology
- Female predominance with bimodal distribution, prepubertal children and postmenopausal females
- Frequency in the U.S. (Int J Womens Dermatol 2020;6:260)
- 0.05% is likely an underestimation
- 0.01% in the pediatric population
Sites
- Anogenital (85%)
- Extragenital (15%), most commonly on back, proximal extremities, chest and thighs (Acta Derm Venereol 2013;93:238)
Pathophysiology / etiology
- Currently unknown etiology (Front Med (Lausanne) 2023;10:1106318)
- Possible genetic predisposition
- Immune mediated Th1 specific IFNγ induced phenotype (Front Med (Lausanne) 2023;10:1106318)
- Circulating IgG autoantibodies against ECM1 (Front Med (Lausanne) 2023;10:1106318)
Clinical features
- White, flat topped papules, plaques or atrophic patches
- May be surrounded by an erythematous to violaceous halo
- Atrophic lesions: skin is smooth, wrinkled and soft
- Itching is frequently severe, especially in anogenital area
- Dysuria, urethral and vaginal discharge, dyspareunia, burning pain, fissuring and erosion may occur
- Obliteration of anatomic structures with loss of labia minora, clitoral hood and urethral meatus
- Perianal and vulvar involvement results in a figure 8 appearance
- Phimosis, paraphimosis and recurrent balanitis are common in men
- Associated with increased risk for genital squamous cell carcinoma (SCC) (Int J Cancer 2017;140:1998)
- Rare reports of pediatric and adult vulvar melanoma arising in association with LS (Pediatr Dermatol 2016;33:e190)
- Can be seen in association with morphea / scleroderma as overlapping lesions
Diagnosis
- Clinical findings are helpful; however, biopsy provides a definitive diagnosis, especially in the following settings
- Clinically equivocal lesions
- Treatment resistant lesions
- Suspicion for malignancy
Prognostic factors
- Early diagnosis, treatment and response to treatment may prevent progression of disease
- Late diagnosis / longstanding lesions, incomplete treatment compliance / response and coexisting neoplasia (VIN) may contribute to an increased risk of SCC, particularly in females (Gynecol Oncol 2020;157:671)
Case reports
- 27 year old man with extragenital lichen sclerosus mimicking cutaneous T cell lymphoma (J Cutan Pathol 2010;37:982)
- 33 year old man with lichen sclerosus along lines of Blaschko (Indian Dermatol Online J 2015;6:342)
- 66 year old woman with a hemorrhagic cutaneous breast lesion (Dermatol Online J 2019;25:13030)
- 67 year old man with a lichen sclerosus associated nevus on the glans penis (JAAD Case Rep 2020;6:323)
Treatment
- High potency topical corticosteroids (first line)
- Topical calcineurin inhibitors
- Intralesional corticosteroids, topical calcipotriol, hydroxychloroquine, cyclosporine, penicillamine, methotrexate and phototherapy (reserved for refractory cases)
- Reference: Front Med (Lausanne) 2023;10:1106318
Gross description
- White, flat topped papules, plaques or atrophic patches
- Erythematous to violaceous halo may be present
- Fissuring and erosion may occur
Microscopic (histologic) description
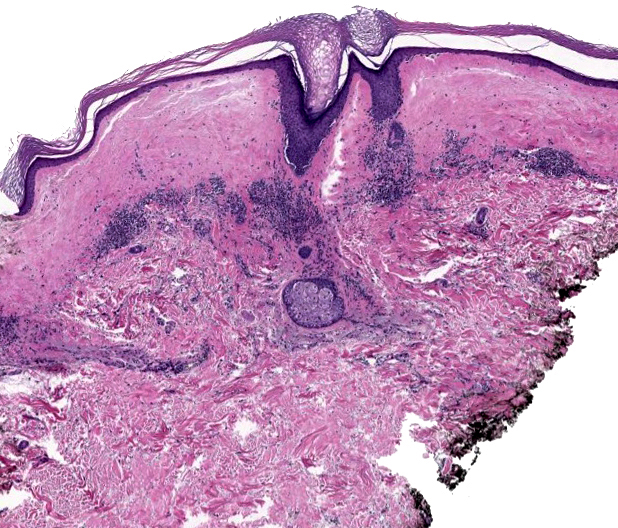
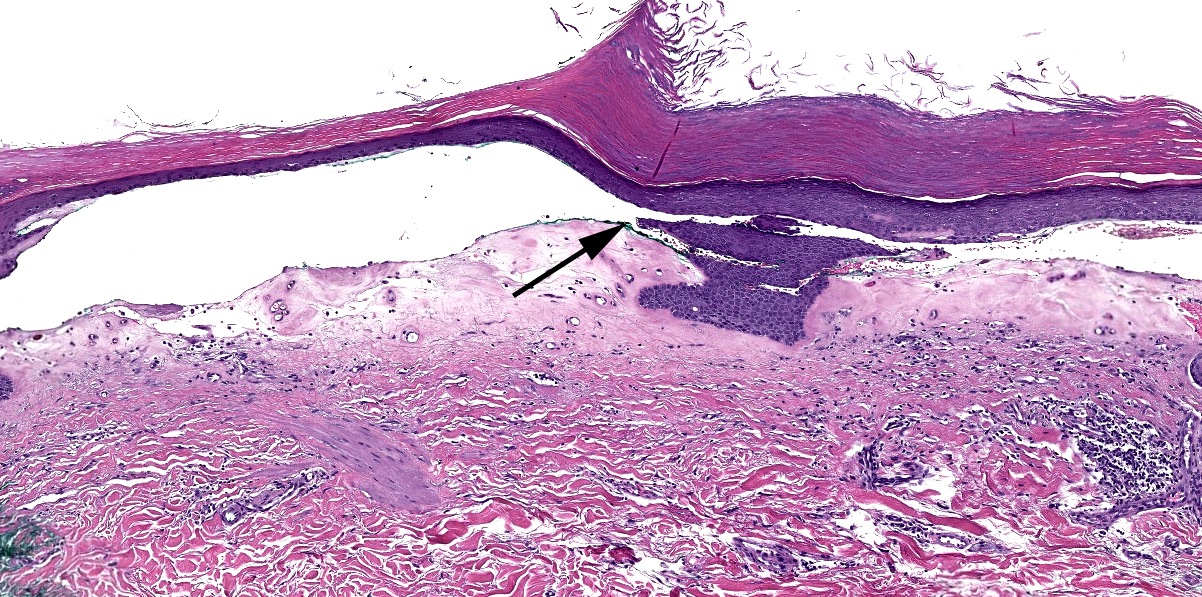
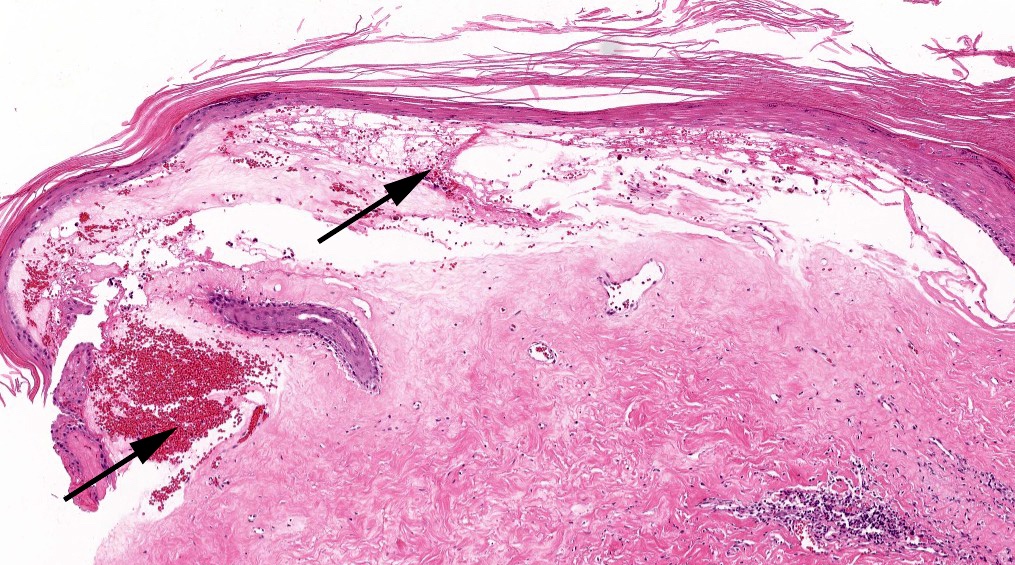
- Low power: striped, trilayered or red, white and blue appearance
- Red: compact orthokeratosis
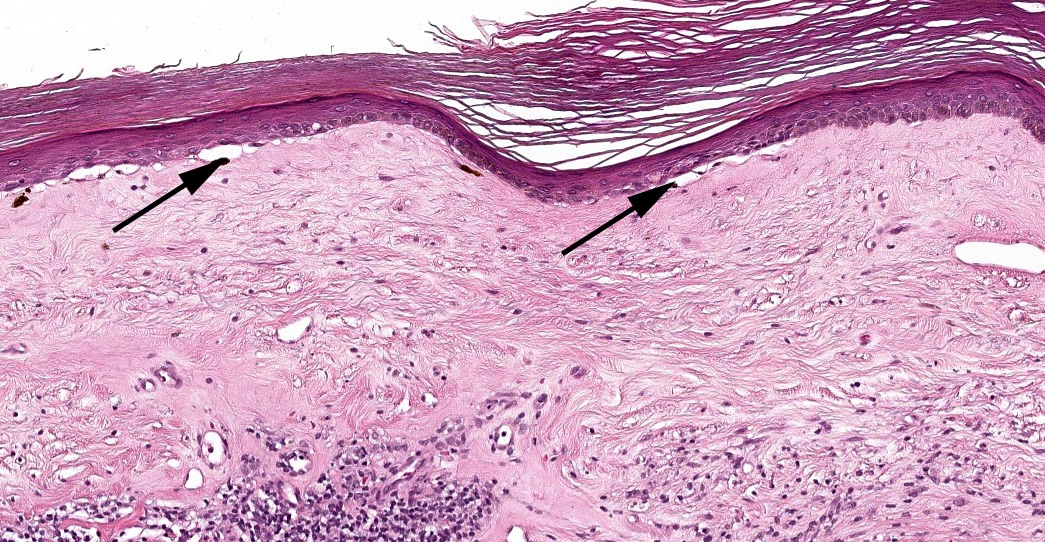
- White: papillary dermal edema / homogenized papillary dermal collagen bundles
- Blue: band-like lymphocytic infiltrate
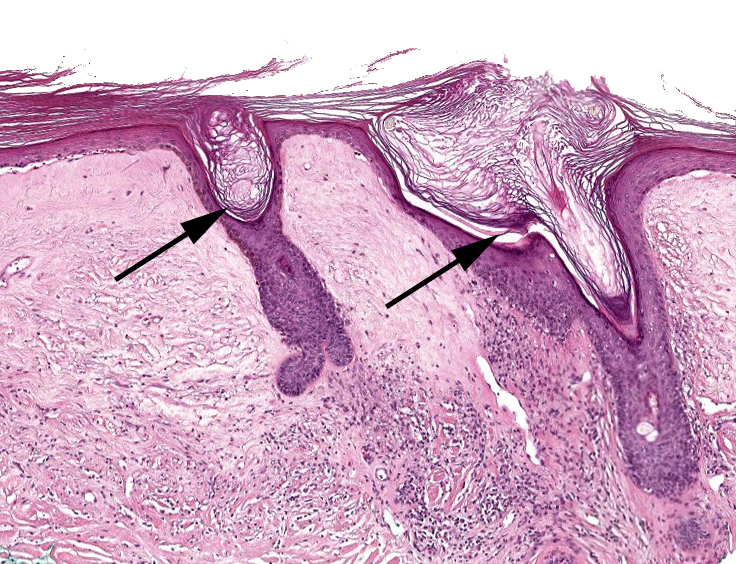
- Early lesions
- Often subtle with changes commonly seen in a periadnexal distribution including follicular hyperkeratosis and hypergranulosis (Histopathology 2005;47:340)
- Variably dense lichenoid or interstitial inflammatory infiltrate
- Homogenization of papillary dermal collagen fibers may be focal
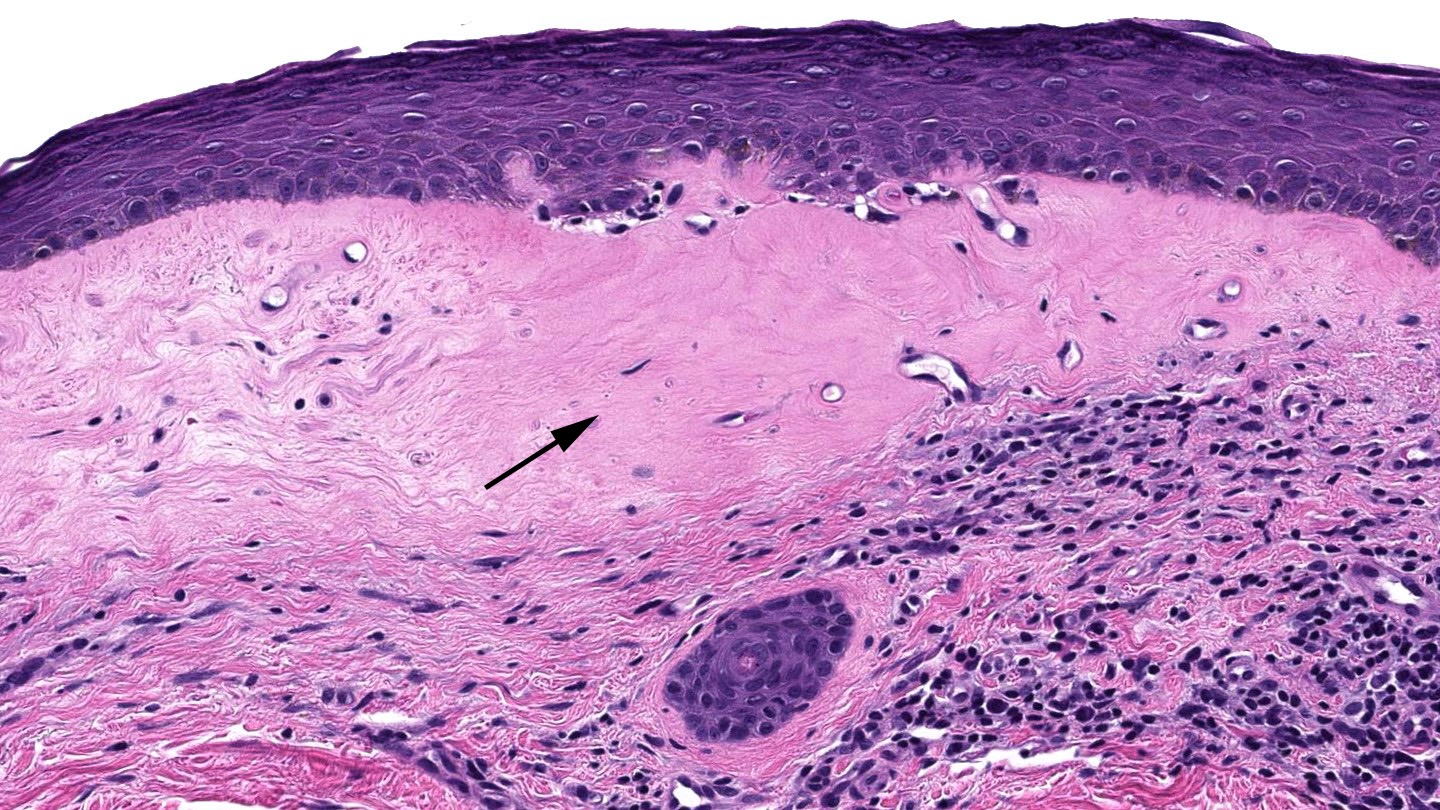
- Established lesions: hyperkeratosis, follicular plugging, epidermal atrophy with loss of rete ridges, basal layer vacuolization, homogenized / sclerotic papillary dermal collagen bundles, a band-like lymphocytic infiltrate and dilated blood vessels
- Acanthosis, dilated blood vessels and eosinophils noted in genital LS (Zhongguo Yi Xue Ke Xue Yuan Xue Bao 2021;43:849)
- Genital LS cases (93.4%) with dense inflammatory infiltrates can demonstrate a mycosis fungoides-like, monoclonal (50%), intraepidermal lymphocytic infiltrate (Am J Surg Pathol 2022;46:83)
Microscopic (histologic) images
Virtual slides
Positive stains
- Immunohistochemical studies generally not needed for diagnosis
Negative stains
- Immunohistochemical studies generally not needed for diagnosis
Videos
Lichen sclerosus in 5 minutes
Lichen sclerosus mimicking mycosis fungoides
Basics of lichen sclerosus
Sample pathology report
- Skin, lower abdomen, shave biopsy:
- Lichen sclerosus (et atrophicus) (see comment)
- Comment: The specimen exhibits compact orthokeratosis, epidermal atrophy, focal basal layer vacuolization, homogenization of papillary dermal collagen fibers and a moderate to dense underlying band-like lymphocytic infiltrate. These findings support the histologic diagnosis.
Differential diagnosis
- Lichen planus:
- Subepidermal band-like lymphocytic infiltrate
- Absence of superficial sclerosis
- Mycosis fungoides, patch / plaque stage:
- Absence of typical histopathologic features of lichen sclerosus
- Monoclonal rearrangement of the T cell receptor gene rearrangement
- Also present in 50% of genital lichen sclerosus (Am J Surg Pathol 2022;46:83)
- Diagnosis of mycosis fungoides in genital skin should be made only upon compelling clinicopathologic criteria
- Vulvar intraepithelial neoplasia (VIN) / penile intraepithelial neoplasia (PeIN):
- Presence of significant keratinocytic atypia
- Abnormal / non-wild type p53 immunostaining
- Lichen simplex chronicus:
- Hypergranulosis
- Epidermal hyperplasia rather than atrophic changes
- Absence of basement membrane degeneration / vacuolization
- Absence of superficial subepidermal sclerosis
- Localized scleroderma / morphea:
- Sparing of the overlying epidermis and superficial dermis
- Involvement of the reticular dermis with extension into the subcutaneous tissue
- Sparse deep periadnexal and perivascular inflammatory infiltrate
- Overlap syndromes can occur
- Chronic radiation dermatitis:
- Radiation induced changes: elastosis, vascular ectasia, enlarged and atypical fibroblasts (radiation fibroblasts)
- Loss of adnexal structures
Board review style question #1
A 67 year old woman presents with a longstanding history of pruritic, atrophic, ivory colored vulvar papules and plaques. A subsequent shave biopsy is performed (see above image). What is the best histologic diagnosis of this lesion?
- Lichen amyloidosis
- Lichen planus
- Lichen sclerosus
- Lichen simplex chronicus
- Vulvar intraepithelial neoplasia
Board review style answer #1
C. Lichen sclerosus. The clinical presentation taken in conjunction with the histologic findings of epidermal atrophy and homogenized papillary dermal collagen fibers with an adjacent focally band-like lymphocytic infiltrate are consistent with lichen sclerosus. Answer B is incorrect because lichen planus, while it generally presents as a band-like inflammatory infiltrate, should not have these changes in the papillary dermal collagen. Answer D is incorrect because lichen simplex chronicus should demonstrate epidermal hyperplasia and lacks the papillary dermal collagen changes and band-like inflammatory infiltrate. Answer A is incorrect because although there is homogenization of the papillary dermal collagen fibers, no amorphous eosinophilic material in the papillary dermis consistent with amyloid and low papillomatous epidermal hyperplasia are seen. Answer E is incorrect because no significant epidermal cytologic atypia is appreciated.
Comment Here
Reference: Lichen sclerosus
Comment Here
Reference: Lichen sclerosus