Management of Subluxated Lenses - KSOS
Management of Subluxated Lenses - KSOS
Management of Subluxated Lenses - KSOS
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
June 2009 S R John et al. - <strong>Management</strong> <strong>of</strong> <strong>Subluxated</strong> <strong>Lenses</strong> 163<br />
<strong>Management</strong> <strong>of</strong> <strong>Subluxated</strong> <strong>Lenses</strong><br />
Dr. Sonia Rani John DNB, Dr. Meena Chakrabarti MS DO DNB, Dr. Arup Chakrabarti MS<br />
Introduction<br />
Subluxation <strong>of</strong> lens signifies partial displacement <strong>of</strong><br />
crystalline lens or cataractous lens from its central<br />
position in the pupillary area.<br />
Fig. 1. A subluxated clear lens<br />
Etiology<br />
Subluxation <strong>of</strong> lens may be congenital or acquired.<br />
Congenital subluxation <strong>of</strong> lens can occur as an isolated<br />
anomaly or associated with heritable disorders. The<br />
acquired subluxation <strong>of</strong> lens may occur due to<br />
hypermaturity <strong>of</strong> cataract, trauma, stretching, pull and<br />
degeneration <strong>of</strong> the zonule 1,2,3,4 .<br />
Signs <strong>of</strong> Zonular damage should be sought in every<br />
patient especially if there is history <strong>of</strong> ocular trauma<br />
or pseudo-exfoliation (PXF).<br />
- Systemic abnormalities associated with zonular<br />
weakness (Marfan’s, Weil Marchesani,<br />
Homocysteinuria) may not always be present.<br />
Hense a loose cataract may be overlooked with<br />
severe surgical consequences. Waneela MV<br />
Margress et al 5 describe 5 subtle signs <strong>of</strong> zonular<br />
Chakrabarti Eye Care Centre, Kochulloor, Trivandrum 695 011<br />
E-mail: tvm_meenarup@sancharnet.in<br />
damage that should be looked for as a warning<br />
sign. These includes<br />
1. Visibility <strong>of</strong> the lens equator during eccentric gaze.<br />
2. Decentered nucleus in primary position<br />
3. Iridolenticular gap.<br />
4. Changes in contour <strong>of</strong> lens periphery.<br />
5. Focal iridodonesis.<br />
OPHTHALMIC<br />
SURGERY<br />
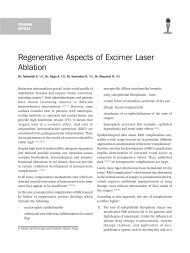
Obvious signs <strong>of</strong> subluxation are less easy to miss and<br />
includes phacodonesis,vitreous prolapse, iridodonesis,<br />
and lens subluxation.<br />
Fig. 2. Anterior segment images demonstrating various<br />
degrees <strong>of</strong> subluxation <strong>of</strong> the crystalline lens<br />
Even without development <strong>of</strong> cataract, subluxation <strong>of</strong><br />
the crystalline lenses can induce significant visual<br />
symptoms such as large refractive errors,<br />
anisometropia, or amlyopia in a child undergoing visual<br />
development.. Historically surgical treatment for<br />
sublaxated lens was undertaken with great caution
164 Kerala Journal <strong>of</strong> Ophthalmology Vol. XXI, No. 2<br />
because <strong>of</strong> attendant complications and poor visual<br />
outcome.<br />
Surgical management was limited to Surgical<br />
iridectomies, Laser iridectomy, discission, or ICCE<br />
Patients who underwent ICCE were either left aphakic<br />
or prescribed aphakic correction ,or CL or were advised<br />
Epikeratophakia. An ACIOL in an older patient was<br />
another option that was considered.These patients<br />
ended up with graft rejection, retinal detachment,<br />
glaucoma and gross visual loss.<br />
Advances that have been made in the surgical<br />
management <strong>of</strong> patients with weak / missing zonules<br />
are SICS, Pars plana lensectomy and aphakic CL wear<br />
or 2 0 ACIOL implantation, suturing PCIOL to ciliary<br />
sulcus / posterior aspect <strong>of</strong> iris 6,7 , introduction <strong>of</strong><br />
CTR(capsular tension rings), MCTRs (modified capsular<br />
tension rings), CTSs (capsular tension segments) 8,9,10,11<br />
and the possibility <strong>of</strong> small incision phacoemulsification<br />
with in the bag IOL implantation.<br />
<strong>Management</strong><br />
Timing <strong>of</strong> surgery is critical and is governed by the<br />
amount <strong>of</strong> subluxation. Children who are in their<br />
visually formative years, need early surgery if they have<br />
a large amount <strong>of</strong> subluxation. Early surgery and visual<br />
rehabilitation prevents development <strong>of</strong> amblyopia or<br />
permits early initation <strong>of</strong> amblyopia therapy. In children<br />
with minimal amounts <strong>of</strong> subluxation that is compatible<br />
with normal visual development can be followed up<br />
without surgical intervention.<br />
An initial assessment <strong>of</strong> the BCVA for distance and near<br />
should be performed. Several attempts at refracting the<br />
child is necessary before deciding whether he is seeing<br />
best with the phakic or aphakic correction. If the<br />
subluxation is not large and there is no eminent danger<br />
<strong>of</strong> the lens dislocating posteriorly or anteriorly<br />
observation with institution <strong>of</strong> amlyopia therapy is all<br />
that is necessary.<br />
If amplyopia cannot be effectively treated by<br />
conventional means such as glasses, contact lens, or<br />
patching, surgical treatment is advisable.<br />
Surgical treatment is also advisable if there is<br />
1. Progressive subluxation.<br />
2. Lens bisects pupil<br />
3. Threathened posterior or anterior dislocation<br />
4. Any case <strong>of</strong> poor visual acuity in an older child or<br />
adult. attributable to subluxated lens.<br />
Preoperative evaluation<br />
Comprehensive preoperative examination is necessary<br />
to increase the chances <strong>of</strong> surgical success.<br />
a) The surgeon should make a note <strong>of</strong> the ‘area <strong>of</strong><br />
zonular weakness “ by drawing it. He should also<br />
i. Characterize the areas <strong>of</strong> zonular weakness in<br />
terms <strong>of</strong> degree <strong>of</strong> involvement.<br />
ii. Location <strong>of</strong> the defect.<br />
iii. Presence / absence <strong>of</strong> vitreous prolapse.<br />
iv. Presence / absence <strong>of</strong> phacodonesis: Phacodonesis<br />
is most dramatic prior to pupillary dilation, as<br />
dilation <strong>of</strong>ten stabilizes the CB and iris, dampening<br />
any iris - lens movement.<br />
A surgeon should be wary <strong>of</strong> inferiorly subluxated lens<br />
as such as sublaxation is <strong>of</strong>ten indicative <strong>of</strong> 360 0 <strong>of</strong><br />
very significant zonular damage combined with the<br />
effect <strong>of</strong> gravity. When the patient is made to lie down<br />
the lens will fall back posteriorly. In this situation it is<br />
unlikely that the surgeon will be able to remove the<br />
lens while preserving the capsular bag for PC IOL<br />
support. PPL should be considered in these cases.<br />
b) Gonioscopy should be performed in older childrenn<br />
to acess for angle recession, synchiae etc if ACIOL<br />
implant is considered.<br />
Patients should be counseled with regards to a sutured<br />
PCIOL / or a CTR.<br />
c) The presence <strong>of</strong> comorbid conditions affecting visual<br />
outcome should be assessed.<br />
d) Evaluation by internists to rule out systemic<br />
associations is also necessary.<br />
e) Discontinuing oral anticoagulants as most if these<br />
patients have asso cardiovascular diseases and may be<br />
on anticoagulant therapy.<br />
A thorough ocular examination including a cycloplegic<br />
refraction, slit-lamp examination and detailed fundus<br />
evaluation should be done to assess the extent <strong>of</strong><br />
subluxation and to plan the treatment approach. The
June 2009 S R John et al. - <strong>Management</strong> <strong>of</strong> <strong>Subluxated</strong> <strong>Lenses</strong> 165<br />
presence <strong>of</strong> iridodonesis, phacodonesis, lens edge and<br />
visible zonules, and relatively deep or an irregularly<br />
deep anterior chamber should be noted. If the lens is<br />
clear, look for irregular red reflex, displacement <strong>of</strong><br />
“Y”sutures, and high refractive error. Intraocular<br />
pressure recording (IOP) and gonioscopy must be<br />
carried out.<br />
Systemic examination is important. A thorough family<br />
history, complete cardiovascular and musculoskeletal<br />
evaluation may be needed in Marfan”s syndrome. In<br />
doubtful cases sodium nitroprusside test for<br />
homocystinuria must be done before subjecting the<br />
patient for general anesthesia.<br />
<strong>Management</strong> <strong>of</strong> Clear <strong>Subluxated</strong> Lens<br />
Conservative Approach<br />
A minimally subluxated crystalline lens requires only<br />
observation and periodic follow-up. If the subluxation<br />
causes visual disturbances due to induced astigmatism<br />
or myopia, the management includes a cycloplegic<br />
refraction and subjectiveverification with prescription<br />
<strong>of</strong> full correction. Examination <strong>of</strong> undilated, aphakic<br />
and phakic portions <strong>of</strong> the pupil should be done to<br />
ascertain whether the patient has got unilateral<br />
diplopia or confusion. Appropriate spectacle correction<br />
with aphakic glasses, contact lenses or prisms is<br />
provided which gives better visual improvement than<br />
phakic correction. Argon or Nd:YAG laser iridoplasty<br />
can be tried to enlarge the aphakic portion <strong>of</strong> pupil.<br />
<strong>Management</strong> <strong>of</strong> <strong>Subluxated</strong> Cataract<br />
Lens extraction via a small incision PE and PCIOL<br />
implantation should be attempted in every case and<br />
the basic surgical principles are described below.<br />
Surgical principles to be understood include<br />
1. Incision should be placed away from area <strong>of</strong> zonular<br />
weakness to help reduce stress on the existing<br />
zonules during PE. Unfortunately majority <strong>of</strong> the<br />
patients have generalized zonular weakness. In<br />
this situation the surgeon should place the incision<br />
in the gradient opposite to the zone <strong>of</strong> maximum<br />
zonular weakness However, the surgeon should<br />
not jeopardize his surgical ability by operating<br />
in a meridian he is uncomfortable with.<br />
2. Surgeon should work through the smallest incision<br />
possible without compromising the ability to<br />
perform necessary maneuvers. This will minimize<br />
fluid egress through the incision and prevent<br />
anterior chamber collapse. The initial AC entry<br />
should be just large enough to introduce a visco<br />
cannula.<br />
3. A generous amount <strong>of</strong> highly retentive viscoelastic<br />
is placed over the area <strong>of</strong> zonular dialysis to help<br />
tamponade the vitreous and to maintain a deep<br />
non collapsingAC.<br />
4. The capsulorhexis is started in an area remote<br />
from the dialysis to help utilize the counter acting<br />
forces <strong>of</strong> the remaining healthy zonules.<br />
5. A second instrument is used for counter traction<br />
or to push the lens into view if it is significantly<br />
decentered under the iris<br />
6. When there is extensive zonular loss or weakness<br />
it may be a good strategy to start the rhexis by<br />
cutting the anterior capsule with a sharp tipped<br />
blade.<br />
7. A rhexis <strong>of</strong> 5.5 mm – 6mm will facilitate all<br />
manipulations <strong>of</strong> the nucleus.<br />
8. Hydrodissection: should be performed carefully<br />
yet thoroughly to maximally free the nucleus<br />
thereby decreasing zonular stress while<br />
manipulating the nucleus.<br />
9. A s<strong>of</strong>t nucleus can be completely prolapsed into<br />
the anterior chamber to simplify removal and<br />
virtually eliminate all zonular stress.<br />
10. Phacoemulsification should be performed using<br />
low vacuum and aspiration settings in order to<br />
keep the bottle height at a minimum, a technique<br />
known as ‘slow-motion Phaco developed by Robert<br />
Osher.<br />
11. Bottle height : it is important to keep the bottle at<br />
an optimum height, neither too high nor too low.<br />
a. Very high bottle height can in turn force fluid<br />
through weak areas <strong>of</strong> the zonules hydrating the<br />
vitreous resulting in positive pressure, anterior<br />
chamber shallowing and vitreous prolapse.<br />
b. Too low bottle height can result in an out flow,<br />
which is greater than inflow again resulting in
166 Kerala Journal <strong>of</strong> Ophthalmology Vol. XXI, No. 2<br />
shallowing <strong>of</strong> anterior chamber, a negative<br />
pressure in AC and further vitreous prolapse as<br />
the anterior segment is less pressurised than the<br />
posterior segment.<br />
12. Divide and or chop technique are preferred in eyes<br />
with zonular weakness. This technique minimises<br />
zonular stress during phacoemulsification if<br />
surgeon is careful to apply equal forces in opposing<br />
directions to avoid displacing the nucleus.<br />
13. “Visco dissect” nuclear halves / quadrants in areas<br />
<strong>of</strong> zonular weakness. The viscoelastic should be<br />
injected below the nuclear fragment and the<br />
capsular bag- lifting the nuclear fragment as well<br />
as expanding and stabilizing the capsular bag.<br />
Additional cortical removal by visco dissection<br />
will limit stress on the remaining zonules during<br />
aspiration <strong>of</strong> cortex.<br />
14. Automated Irrigation and Aspiration device is not<br />
preferred for cortex removal as it can hydrate<br />
vitreous and increase vit prolapse. Manually<br />
aspirate with a 24/ 27 G canula striping cortex in<br />
a tangential manner instead <strong>of</strong> radially to limit<br />
stress on zonules. A ‘J’ cannula can be used for<br />
sub incisional cortex .Ensure removal <strong>of</strong> all<br />
vitreous from the anterior chamber if it is present.<br />
Use ‘Dry vitrectomy’ with automated vitrector<br />
after filling anterior chamber with viscoelastics.<br />
For significant vitreous loss a bimanual vitrectomy<br />
should be performed.<br />
IOL placement options<br />
1. The surgeon should decide if it is safe to use an<br />
ACIOL or PCIOL.<br />
2. If an ACIOL is used the remnants <strong>of</strong> the capsular<br />
bag should be removed to prevent contraction and<br />
opacification.<br />
3. If the surgeon uses a PCIOL it should be either<br />
a. Sutured to the scleral wall or<br />
b. Placed in the capsular bag<br />
Ciliary sulcus placement <strong>of</strong> PCIOL without suture<br />
fixation in an eye with significant zonular compromise<br />
is not recommended.<br />
Placement <strong>of</strong> PCIOL into the capsular bag<br />
1. Placement <strong>of</strong> PCIOL into the capsular bag is<br />
challenging when there is significant zonular<br />
weakness as one must achieve IOL centration, and<br />
maximize long term stability.<br />
2. Use <strong>of</strong> 6 mm optic diametre IOL decreases the<br />
chances <strong>of</strong> undesirable edge - glare symptoms<br />
should lens decentration occur post operatively.<br />
Haptic configuration designed for broad contact<br />
with equatorial capsular bag increases the chances<br />
<strong>of</strong> long term centration. Use <strong>of</strong> silicone plate haptic<br />
IOL. should be avoided in the presence <strong>of</strong> zonular<br />
dialysis as there is greater chance <strong>of</strong> capsular<br />
contraction and decentration.<br />
3. Insertion <strong>of</strong> CTR to provide 360 0 capsular bag<br />
expansion and greater stabilization.<br />
4. If the ZD is located at the incision site, lens<br />
placement is more difficult.<br />
a. One Option is to first place the entire lens into<br />
the AC. Then using a two handed technique, the<br />
superior haptic is inserted into the capsular bag<br />
followed by a similar maneuvre for the inferior<br />
haptic.<br />
5. Orientation <strong>of</strong> the IOL: There are 2 schools <strong>of</strong><br />
thought.<br />
a. Orienting the IOL in a plane parallel to the zonular<br />
dialysis (ZD) in order to take advantage <strong>of</strong> the<br />
remaining intact zonules. This orientation will<br />
provide optimum support but may induce ovaling<br />
<strong>of</strong> the capsular bag and an increased risk <strong>of</strong><br />
postoperative decentration.<br />
b. Placing one haptic in area <strong>of</strong> ZD will ensure<br />
stretching <strong>of</strong> the bag and decrease ovaling.<br />
However it should be borne in mind that only one<br />
haptic is adequately supported.<br />
It is recommended to orient the haptics in whichever<br />
axis that provides the best centration intraoperatively.<br />
This is accomplished by careful rotation <strong>of</strong> PCIOL.<br />
Capsular Tension Ring (CTRs)<br />
Drs Witschel and Legler (1993) from Germany<br />
demonstrated that CTRs could provide both<br />
intraoperative and postoperative stabilization <strong>of</strong>
June 2009 S R John et al. - <strong>Management</strong> <strong>of</strong> <strong>Subluxated</strong> <strong>Lenses</strong> 167<br />
the capsular bag. Produced by Morcher Gmbh, in<br />
Stuttgarf, Germany and made <strong>of</strong> polymethyl<br />
methacrylate (PMMA), this ring can be inserted<br />
into capsular bag at any point after a continuous<br />
curvilinear capsulorhexis has been completed.<br />
Use <strong>of</strong> CTR is contra indicated if a CCC is not<br />
attained or if a posterior capsular rent occurs.<br />
In eyes with pr<strong>of</strong>ound zonular compromise or lens<br />
subluxation may not achieve adequate<br />
stabilization or centration despite CTR placement.<br />
Long term stability even in presence <strong>of</strong> CTR is doubtful<br />
in eyes with progressive zonular weakness such as<br />
Marfans, PXF etc. Phacoemulsification with the proper<br />
use <strong>of</strong> endocapsular device can give excellent results<br />
in patients with subluxated cataracts<br />
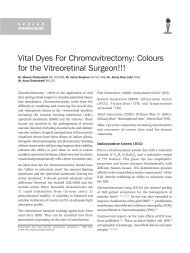
Fig 3. Capsular tension rings <strong>of</strong> commonly used sizes ,Geuder<br />
injector and intraoperative still photography to<br />
demonstrate CTR insertion<br />
Step1: Injection <strong>of</strong> VE under the surface <strong>of</strong> the residual<br />
anterior capsular ring to create a path for the CTR.<br />
Viscoelastic agents dissect peripheral cortex away from<br />
the capsular fornices and make up cortex entrapment<br />
by CTR less likely.<br />
Step 2 :<br />
a) CTR is introduced either using a smooth forceps<br />
through the main wound or a paracentesis or by<br />
b) Using a CTR injector / CTR shooter (Geuder)<br />
Step 3 : In eyes where CTR is introduced prior to<br />
phacoemulsification a safety suture is looped through<br />
the leading eyelet and is allowed to trial out <strong>of</strong> the eye<br />
Fig. 4. Intraoperative stillphotography demonstrating CTR<br />
insertion<br />
at the main incision during PE and cortical aspiration.<br />
This guiding suture is used to retrieve the CTR from<br />
the eye should a posterior capsular rent occur during<br />
phacoemulsification or cortex removal. If the procedure<br />
is uneventful the suture is cut and removed.<br />
Standard capsular tension ring<br />
Credit goes to Hara and Yamada 12 for introducing<br />
endocapsular ring in the year 1991 for maintenance <strong>of</strong><br />
the circular diameter <strong>of</strong> capsular bag. Later the device<br />
Fig. 5. Standard capsular tension ring<br />
was further refined and modified for managing severe<br />
degree <strong>of</strong> subluxated lenses 12-16 .<br />
The standard CTR in made <strong>of</strong> polymethyl<br />
methacrylate(PMMA) material and has an oval shaped<br />
cross section with eyelets at both free ends (Fig.5).<br />
It is a compressible circular ring with two smooth edged<br />
end terminals.<br />
CTR is manufactured by Morcher GmbH (Struttgarf,<br />
Germany) and Ophtek (Groningen, The Netherlands)
168 Kerala Journal <strong>of</strong> Ophthalmology Vol. XXI, No. 2<br />
Fig. 6. Morcher CTRs<br />
Type 14, MR – 1400,<br />
For Normal Eyes<br />
Expanded 12.3mm,<br />
Compressibility 10.0mm,<br />
Axial Length < 24mm<br />
Type 14A, MR – 1410,<br />
For Highly Myopic Eyes<br />
Expanded 14.5mm,<br />
Compressibility 12.0mm,<br />
Axial Length < 28mm<br />
Type 14C, MR – 1420,<br />
For Normal or Myopic Eyes<br />
Expanded 13.0mm,<br />
Compressibility 11.0mm,<br />
Axial Length 24 - 28mm<br />
and is US-FDA approved. The Morcher ring, also known<br />
as Reform ring, comes in three different sizes based on<br />
the uncompressed diameter (Fig.6).<br />
Capsular ring size<br />
Selection <strong>of</strong> CTR size is based on capsular bag<br />
dimensions. A large capsular bag usually requires a<br />
larger ring; 13mm ring is being most commonly used.<br />
White to white corneal measurement and axial length<br />
can be used as a rough guide in the selection <strong>of</strong> CTR. It<br />
would be appropriate to use a larger CTR in adults with<br />
highly myopic eyes.<br />
Step 4: Placement <strong>of</strong> IOL in the bag and has the CTR is<br />
no different than routine cases, infact it may be even<br />
easier as the bag is better supported.<br />
Step 5: Suturing the CTR to Scleral wall for support.<br />
although it works well involves risk <strong>of</strong> rupturing<br />
the capsular bag since it is under stretch due to<br />
presence <strong>of</strong> CTR.<br />
Vladimic Pfizer’s technique involves needle passage thro<br />
a small peripheral capsulorhexis. However the integrity<br />
<strong>of</strong> the capsular bag is violated and the risk <strong>of</strong> rupture is<br />
present.<br />
In more severe subluxation, modified CTR, like Cionni’s<br />
M-CTR with one or two eyelets attached to the central<br />
ring is used and a posterior chamber IOL (PCIOL)<br />
placed in-the-bag.<br />
Robert Cionni:s Modified CTR (MCTR) 8,9,10 has an<br />
unique fixation hooklet designed for scleral fixation<br />
without violating the integrity <strong>of</strong> capsular bag. The<br />
fixation hook courses anteriorly and centrally in a<br />
second plane, wraps around the capsulorhexis edge<br />
and rests on the residual anterior capsular rim.<br />
Modified capsular tension ring (M- CTR)<br />
The standard CTR is unable to provide adequate<br />
intraoperative support and centration <strong>of</strong> the bag in<br />
Ring with single eyelet Ring with double eyelets<br />
Fig. 7. Cionni’s modified capsular tension ring<br />
a) Robert Osher has desired a technique <strong>of</strong> suturing<br />
the CTR to the scleral wall by straddling the CTR<br />
with 10 0 prolene double suture. This technique Fig. 8. Cionni’s modified Capsular Tension Segments
June 2009 S R John et al. - <strong>Management</strong> <strong>of</strong> <strong>Subluxated</strong> <strong>Lenses</strong> 169<br />
grossly subluxated cataracts or lenses. Cionni 5<br />
developed the modified CTR (M-CTR) (Morcher –<br />
GmbH) called Cionni ring in the year 1998. This ring<br />
provides a solution to extensive zonular deficiency or<br />
damage or progressive zonular damage by allowing the<br />
surgeon to anchor the capsular bag to the sclera.<br />
3 modules are currently available.<br />
Model 1 L : Single fixation hook distant from insertion<br />
end <strong>of</strong> the ring.<br />
Model 2 C: Single fixation hook near insertion end <strong>of</strong><br />
the ring.<br />
Model 2 L: has 2 fixation hooks which is very useful in<br />
patients with significant zonular weakness and may be<br />
the ring <strong>of</strong> choice in patients with progressive zonular<br />
weakness as in Marfan’s Syndrome.<br />
The Cionni’s modified ring has an open ring design<br />
with one (model I-L or I-R) or two (model 2-L)<br />
fixation eyelets attached to the central ring (Fig 7).<br />
The eyelet allows the ring to be sutured to the sclera.<br />
It protrudes 0.25mm forward from the body <strong>of</strong> the<br />
ring and then sits anterior to the anterior capsular rim<br />
and allows maintenance <strong>of</strong> capsular bag integrity on<br />
suturing to the sclera. A 9.0 prolene is preferred over<br />
10.0 prolene as the incidence <strong>of</strong> breakage is less with<br />
the former. An adequately sized rhexis is essential to<br />
prevent iris chaffing, pigment dispersion and chronic<br />
uveitis.<br />
An eccentric rhexis has to be performed in order to be<br />
certain that after the bag is recentred, the capsulorhexis<br />
opening is recentered as well.<br />
Fig. 9. Capsular tension segment<br />
Capsular tension segment<br />
Capsular tension segment (CTS) is a partial ring <strong>of</strong><br />
90-120 circumference, and is made <strong>of</strong> PMMA<br />
(Fig. 8 & 9). It has a radius <strong>of</strong> 5mm and an anteriorly<br />
positioned fixation eyelet like M- CTR. This was<br />
designed by Ahmed 17 . and was manufactured by<br />
Morcher GmbH. CTS is useful for cases with pr<strong>of</strong>ound<br />
zonular insufficiency. The CTS provides support in the<br />
transverse plane, when sutured to the scleral wall.<br />
When circumferential support is needed, a CTR may<br />
be implanted in conjunction with an already positioned<br />
CTS. The CTS in available in 3 sizes having radus <strong>of</strong><br />
curvature <strong>of</strong> 4.5 mm , 5 mm and 5.5 mm.<br />
The choice <strong>of</strong> endocapsular support device depends<br />
mainly on the nature <strong>of</strong> zonular weakness, degree <strong>of</strong><br />
zonular loss, and the extent <strong>of</strong> zonular instablity. CTRs<br />
are indicated in cases <strong>of</strong> mild, generalized zonular<br />
weakness or in small localized zonular dialysis <strong>of</strong> less<br />
than 3-4 clock hours. In more advanced or progressive<br />
Table 1: Indications <strong>of</strong> capsular tension ring, modified-capsular tension ring and capsular tension segment<br />
CTR M-CTR CTS<br />
Requires continuous curvilinear capsulorhexis Yes Yes No<br />
May be placed prior to lens removal With difficulty With difficulty Yes<br />
Use with anterior capsule tear No No Yes<br />
Use with posterior capsule rent No No Yes<br />
Use with large zonular dialysis (more than 8 clock hours) No Yes Yes<br />
( multiple segments)<br />
Use in progressive zonulysis No Yes Yes<br />
Allow for suture fixation to sclera No Yes Yes<br />
May be easily removed from eye if needed No No Yes<br />
Cortical removal difficulty Yes Yes No<br />
CTR: capsular tension ring, M-CTR: modified-capsular tension ring, CTS: capsular tension segment
170 Kerala Journal <strong>of</strong> Ophthalmology Vol. XXI, No. 2<br />
Fig. 10.Successful outcome <strong>of</strong> surgery in a case <strong>of</strong> subluxated<br />
Lens<br />
cases <strong>of</strong> zonular instability, the Cionni M- CTR or the<br />
CTS is indicated. Indications <strong>of</strong> CTR, M-CTR and CTS<br />
are given in Table 1.<br />
Closed chamber endocapsular phacoemulsification<br />
combined with ECR, in patients with mild to moderate<br />
subluxation <strong>of</strong> lens not associated with complications<br />
such as secondary glaucoma and retinal detachment,<br />
<strong>of</strong>ten gives encouraging visual results. The implantation<br />
<strong>of</strong> ECR has provided safety and efficiency during<br />
phacoemulsification and IOL implantation, significantly<br />
reduced the rate <strong>of</strong> complications and overall improved<br />
visual results.<br />
References<br />
1. Jensen A, Cross H. Surgical Tratment <strong>of</strong> dislocated<br />
lenses in Marfan’s Syndrome and homocystinuria. Trans<br />
An Acad Ophthalmol Otolaryngol 76:1491-1499, 1972.<br />
2. Varga.B The result <strong>of</strong> my operations improving visual<br />
acuity <strong>of</strong> ectopialentis Ophthalmologica 162:98-110,<br />
1971.<br />
3. Maumenee IH. The eye in Marfan’s Syndrome. Trans<br />
Am Acard Ophthalmol Soc 79:684- 733, 1981.<br />
4. Straatsma B, Allen.R, Petit.T et al. Subluxation <strong>of</strong> lens<br />
with iris photocoagulation. Am.J.Ophthalmol 61:1312-<br />
1324, 1966.<br />
5. Daniella.M.V, Marques, Frederio.F,Marques, Robert<br />
H.Osher.J.Cataract Refract Surg 2004;30:1295-1299<br />
6. Gimbel H, Condon. G et al. Late in the bag IOL<br />
dislocation; Incidence, prevention and management. J.<br />
Cataract.Refract.Srug. 11:2193-2204, 2005.<br />
7. Zetterstorm C, Landvall A et al. Sulcus fixation with<br />
out capsular support in children. J..Cataract Refract<br />
Surg 25:776-781, 1999.<br />
8. Cionni. R, Osher.R et al. Endocapsular ring approach<br />
to the sublaxated cataractors lens. J CRS 21:245-249,<br />
1995.<br />
9. Cionni.R, Osher.R. <strong>Management</strong> <strong>of</strong> pr<strong>of</strong>ound zonular<br />
dialysis or weakness with a new endocapsular ring<br />
designed for SF. JCRS 10:1299-1306,1998.<br />
10. Cionni.R, Osher.R. et al. MCTRS for patients with<br />
congenital loss <strong>of</strong> zonular support. JCRS, 9:1668-1673,<br />
2003.<br />
11. Hasanee.K, Butter M et al, Ahmed I et al. Capsular<br />
Tension rings and retinal devices: Current Concepts.<br />
Current Opinion Ophthalmol 17:31-41; 2006.<br />
12. Hara T, Yamada Y. “Equator ring” for maintenance <strong>of</strong><br />
the completely circular contour <strong>of</strong> the capsular<br />
equator after cataract removal. Ophthalmic Surg 1991;<br />
22(6):358 – 9.<br />
13. Nagamoto T, Bissen Miyajima H. A Ring to support the<br />
capsular bag after continuous curvilinear<br />
14.<br />
capsulorrhexis. J. Cataract Refract Surg 1994; 20(4):<br />
417 – 20.<br />
Menapace R, Findl O, Georgopoulus M. The capsular<br />
tension ring: designs, applications and techniques. J<br />
Cataract Refract Surg 2000; 26(6): 868 – 912. Review.<br />
15. Vaas C, Menapace R, Findl O. Prediction <strong>of</strong><br />
pseudophakic capsular bag diameter based on biometric<br />
variables. J. Cataract Refract Surg 1999; 25(10): 1376-<br />
81.<br />
16. Osher RH ; History and experience with capsular tension<br />
rings. Cataract Refract Surg Today 2005; 1-5.<br />
17. Ahmed IK, Crandall AS. Ab externo fixation <strong>of</strong> Cionni<br />
modified capsular tension ring. J Cataract Refract Surg<br />
2001;97: 977-81.<br />
18. Praveen MR, Vasavada AR, Singh A. Phacoemulsification<br />
in subluxated cataract. Ind J Ophthalmol 2003;51:147-<br />
54.<br />
19. Cionni RJ, Watanabe TM. Congenitalsubluxation <strong>of</strong> the<br />
crystalline lens and the surgical treatment. In: Cataract<br />
Surgery in Complicated Cases. Buratto L, Osher RH,<br />
Masket S. (Eds).Thor<strong>of</strong>are, Slack Inc, 2000,15-22.<br />
20. Santoro S, Carmela S, Cascella MC, et al. <strong>Subluxated</strong><br />
lens: phacoemulsification with iris hook. J Cataract<br />
Refract Surg 2003;29:2269-73.<br />
21. Chang DF. Capsular tension rings versus capsular<br />
retractors. Cataract Refract Surg Today 2004 Jan, 38-41.<br />
22. Dieticin TS, Jacobi PC, Konen W, et al. Complications<br />
<strong>of</strong> endocapsular tension ring implanted in child with<br />
Marfan’s syndrome. J Cataract Refract Surg 2000;<br />
26:937-40.<br />
23. Bahar I, Kaiserman I, Rootman D. Cionni endocapsular<br />
ring implantation in Marfan’s syndrome. Br J<br />
Ophthalmol 2007.<br />
24. Hara T, Hara T, Hara T. Preventing posterior capsule<br />
opacification with an endocapsular equator ring in<br />
young human eye. Arch Ophthalmol 2007,125:483-86.