Abstract
Purpose
Cancer-related fatigue (CRF) is a common and distressing symptom of cancer that may persist for years following treatment completion. However, little is known about the pathophysiology of CRF. Using a comprehensive group of gold-standard physiological and psychosocial assessments, this study aimed to identify correlates of CRF in a heterogenous group of cancer survivors.
Methods
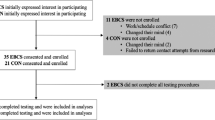
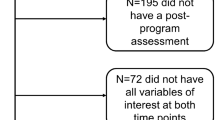
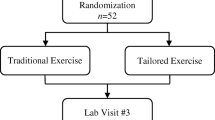
Using a cross-sectional design to determine the physiological and psychosocial correlates of CRF, ninety-three cancer survivors (51 fatigued, 42 non-fatigued) completed assessments of performance fatigability (i.e. the decline in muscle strength during cycling), cardiopulmonary exercise testing, venous blood samples for whole blood cell count and inflammatory markers and body composition. Participants also completed questionnaires measuring demographic, treatment-related, and psychosocial variables.
Results
Performance fatigability, time-to-task-failure, peak oxygen uptake (V̇O2peak), tumor necrosis factor-α (TNF-α), body fat percentage, and lean mass index were associated with CRF severity. Performance fatigability, V̇O2peak, TNF-α, and age explained 35% of the variance in CRF severity. Those with clinically-relevant CRF reported more pain, more depressive symptoms, less perceived social support, and were less physically active than non-fatigued cancer survivors.
Conclusions
The present study utilised a comprehensive group of gold-standard physiological and psychosocial assessments and the results give potential insight into the mechanisms underpinning the association between physical inactivity, physical deconditioning and CRF.
Implications for Cancer Survivors
Given the associations between CRF and both physiological and psychosocial measures, this study identifies targets that can be measured by rehabilitation professionals and used to guide tailored interventions to reduce fatigue.




Similar content being viewed by others
Data availability
Data available upon request.
Code availability
Not applicable.
References
Berger AM, Mooney K, Alvarez-Perez A, Breitbart WS, Carpenter KM, Cella D, et al. Cancer-Related Fatigue, Version 2.2015. J Natl Compr Canc Netw JNCCN. 2015;13(8):1012–39. https://doi.org/10.6004/jnccn.2015.0122.
Lawrence DP, Kupelnick B, Miller K, Devine D, Lau J. Evidence report on the occurrence, assessment, and treatment of fatigue in cancer patients. J Natl Cancer Inst Monogr. 2004;32:40–50. https://doi.org/10.1093/jncimonographs/lgh027.
Curt GA, Breitbart W, Cella D, Groopman JE, Horning SJ, Itri LM, et al. Impact of cancer-related fatigue on the lives of patients: new findings from the Fatigue Coalition. Oncologist. 2000;5(5):353–60. https://doi.org/10.1634/theoncologist.5-5-353.
Goedendorp MM, Gielissen MF, Verhagen CA, Bleijenberg G. Development of fatigue in cancer survivors: a prospective follow-up study from diagnosis into the year after treatment. J Pain Symptom Manage. 2013;45(2):213–22. https://doi.org/10.1016/j.jpainsymman.2012.02.009.
Jones JM, Olson K, Catton P, Catton CN, Fleshner NE, Krzyzanowska MK, et al. Cancer-related fatigue and associated disability in post-treatment cancer survivors. J Cancer Surviv. 2016;10(1):51–61. https://doi.org/10.1007/s11764-015-0450-2.
Bower JE, Ganz PA, Desmond KA, Rowland JH, Meyerowitz BE, Belin TR. Fatigue in Breast Cancer Survivors: Occurrence, Correlates, and Impact on Quality of Life. J Clin Oncol. 2000;18(4):743. https://doi.org/10.1200/jco.2000.18.4.743.
Goldstein D, Bennett BK, Webber K, Boyle F, de Souza PL, Wilcken NR, et al. Cancer-related fatigue in women with breast cancer: outcomes of a 5-year prospective cohort study. J Clin Oncol. 2012;30(15):1805–12. https://doi.org/10.1200/jco.2011.34.6148.
Islam T, Dahlui M, Majid HA, Nahar AM, Mohd Taib NA, Su TT. Factors associated with return to work of breast cancer survivors: a systematic review. BMC Public Health. 2014;14(Suppl 3):S8. https://doi.org/10.1186/1471-2458-14-s3-s8.
Miller KD, Nogueira L, Mariotto AB, Rowland JH, Yabroff KR, Alfano CM, et al. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. 2019;69(5):363–85. https://doi.org/10.3322/caac.21565.
McNeely ML, Courneya KS. Exercise programs for cancer-related fatigue: evidence and clinical guidelines. J Natl Compr Canc Netw JNCCN. 2010;8(8):945–53. https://doi.org/10.6004/jnccn.2010.0069.
Carpenter JS, Elam JL, Ridner SH, Carney PH, Cherry GJ, Cucullu HL. Sleep, fatigue, and depressive symptoms in breast cancer survivors and matched healthy women experiencing hot flashes. Oncol Nurs Forum. 2004;31(3):591–5598. https://doi.org/10.1188/04.onf.591-598.
Kuhnt S, Ernst J, Singer S, Rüffer JU, Kortmann RD, Stolzenburg JU, et al. Fatigue in cancer survivors–prevalence and correlates. Onkologie. 2009;32(6):312–7. https://doi.org/10.1159/000215943.
Servaes P, Verhagen C, Bleijenberg G. Fatigue in cancer patients during and after treatment: prevalence, correlates and interventions. Eur J Cancer. 2002;38(1):27–43. https://doi.org/10.1016/s0959-8049(01)00332-x.
Beck SL, Dudley WN, Barsevick A. Pain, sleep disturbance, and fatigue in patients with cancer: using a mediation model to test a symptom cluster. Oncol Nurs Forum. 2005;32(3):542. https://doi.org/10.1188/04.onf.e48-e55.
Martin T, Twomey R, Medysky ME, Temesi J, Culos-Reed SN, Millet GY. The Relationship between Fatigue and Actigraphy-Derived Sleep and Rest-Activity Patterns in Cancer Survivors. Curr Oncol. 2021;28(2):1170–82. https://doi.org/10.3390/curroncol28020113.
Servaes P, Verhagen S, Bleijenberg G. Determinants of chronic fatigue in disease-free breast cancer patients: a cross-sectional study. Ann Oncol. 2002;13(4):589–98. https://doi.org/10.1093/annonc/mdf082.
Gielissen MF, Verhagen S, Witjes F, Bleijenberg G. Effects of cognitive behavior therapy in severely fatigued disease-free cancer patients compared with patients waiting for cognitive behavior therapy: a randomized controlled trial. J Clin Oncol. 2006;24(30):4882–7. https://doi.org/10.1200/jco.2006.06.8270.
Corbett TK, Groarke A, Devane D, Carr E, Walsh JC, McGuire BE. The effectiveness of psychological interventions for fatigue in cancer survivors: systematic review of randomised controlled trials. Syst Rev. 2019;8(1):324. https://doi.org/10.1186/s13643-019-1230-2.
Saligan LN, Olson K, Filler K, Larkin D, Cramp F, Yennurajalingam S, et al. The biology of cancer-related fatigue: a review of the literature. Support Care Cancer. 2015;23(8):2461–78. https://doi.org/10.1007/s00520-015-2763-0.
Neil SE, Klika RJ, Garland SJ, McKenzie DC, Campbell KL. Cardiorespiratory and neuromuscular deconditioning in fatigued and non-fatigued breast cancer survivors. Support Care Cancer. 2013;21(3):873–81. https://doi.org/10.1007/s00520-012-1600-y.
Yavuzsen T, Davis MP, Ranganathan VK, Walsh D, Siemionow V, Kirkova J, et al. Cancer-related fatigue: central or peripheral? J Pain Symptom Manage. 2009;38(4):587–96. https://doi.org/10.1016/j.jpainsymman.2008.12.003.
Kilgour RD, Vigano A, Trutschnigg B, Hornby L, Lucar E, Bacon SL, et al. Cancer-related fatigue: the impact of skeletal muscle mass and strength in patients with advanced cancer. J Cachexia Sarcopenia Muscle. 2010;1(2):177–85. https://doi.org/10.1007/s13539-010-0016-0.
Enoka RM, Duchateau J. Translating Fatigue to Human Performance. Med Sci Sports Exerc. 2016;48(11):2228–38. https://doi.org/10.1249/mss.0000000000000929.
Kisiel-Sajewicz K, Davis MP, Siemionow V, Seyidova-Khoshknabi D, Wyant A, Walsh D, et al. Lack of muscle contractile property changes at the time of perceived physical exhaustion suggests central mechanisms contributing to early motor task failure in patients with cancer-related fatigue. J Pain Symptom Manage. 2012;44(3):351–61. https://doi.org/10.1016/j.jpainsymman.2011.08.007.
Twomey R, Aboodarda SJ, Kruger R, Culos-Reed SN, Temesi J, Millet GY. Neuromuscular fatigue during exercise: Methodological considerations, etiology and potential role in chronic fatigue. Neurophysiol Clin. 2017;47(2):95–110. https://doi.org/10.1016/j.neucli.2017.03.002.
Andrykowski MA, Donovan KA, Laronga C, Jacobsen PB. Prevalence, predictors, and characteristics of off-treatment fatigue in breast cancer survivors. Cancer. 2010;116(24):5740–8. https://doi.org/10.1002/cncr.25294.
Reinertsen KV, Cvancarova M, Loge JH, Edvardsen H, Wist E, Fosså SD. Predictors and course of chronic fatigue in long-term breast cancer survivors. J Cancer Surviv. 2010;4(4):405–14. https://doi.org/10.1007/s11764-010-0145-7.
Greenberg DB, Gray JL, Mannix CM, Eisenthal S, Carey M. Treatment-related fatigue and serum interleukin-1 levels in patients during external beam irradiation for prostate cancer. J Pain Symptom Manage. 1993;8(4):196–200. https://doi.org/10.1016/0885-3924(93)90127-h.
Lutgendorf SK, Weinrib AZ, Penedo F, Russell D, DeGeest K, Costanzo ES, et al. Interleukin-6, cortisol, and depressive symptoms in ovarian cancer patients. J Clin Oncol. 2008;26(29):4820–7. https://doi.org/10.1200/jco.2007.14.1978.
Bower JE, Ganz PA, Irwin MR, Kwan L, Breen EC, Cole SW. Inflammation and behavioral symptoms after breast cancer treatment: do fatigue, depression, and sleep disturbance share a common underlying mechanism? J Clin Oncol. 2011;29(26):3517–22. https://doi.org/10.1200/jco.2011.36.1154.
Collado-Hidalgo A, Bower JE, Ganz PA, Cole SW, Irwin MR. Inflammatory biomarkers for persistent fatigue in breast cancer survivors. Clin Cancer Res. 2006;12(9):2759–66. https://doi.org/10.1158/1078-0432.ccr-05-2398.
Bower JE, Ganz PA, Aziz N, Fahey JL. Fatigue and proinflammatory cytokine activity in breast cancer survivors. Psychosom Med. 2002;64(4):604–11. https://doi.org/10.1097/00006842-200207000-00010.
Kisiel-Sajewicz K, Siemionow V, Seyidova-Khoshknabi D, Davis MP, Wyant A, Ranganathan VK, et al. Myoelectrical manifestation of fatigue less prominent in patients with cancer related fatigue. PLoS ONE. 2013;8(12): e83636. https://doi.org/10.1371/journal.pone.0083636.
Twomey R, Martin T, Temesi J, Culos-Reed SN, Millet GY. Tailored exercise interventions to reduce fatigue in cancer survivors: study protocol of a randomized controlled trial. BMC Cancer. 2018;18(1):757. https://doi.org/10.1186/s12885-018-4668-z.
Veni T, Boyas S, Beaune B, Bourgeois H, Rahmani A, Landry S, et al. Handgrip fatiguing exercise can provide objective assessment of cancer-related fatigue: a pilot study. Support Care Cancer. 2019;27(1):229–38. https://doi.org/10.1007/s00520-018-4320-0.
Bower JE. Cancer-related fatigue: links with inflammation in cancer patients and survivors. Brain Behav Immun. 2007;21(7):863–71. https://doi.org/10.1016/j.bbi.2007.03.013.
Brown LF, Kroenke K. Cancer-related fatigue and its associations with depression and anxiety: a systematic review. Psychosomatics. 2009;50(5):440–7. https://doi.org/10.1176/appi.psy.50.5.440.
Oh HS, Seo WS. Systematic review and meta-analysis of the correlates of cancer-related fatigue. Worldviews Evid Based Nurs. 2011;8(4):191–201. https://doi.org/10.1111/j.1741-6787.2011.00214.x.
Bower JE, Ganz PA, Desmond KA, Rowland JH, Meyerowitz BE, Belin TR. Fatigue in breast cancer survivors: occurrence, correlates, and impact on quality of life. J Clin Oncol. 2000;18(4):743–53. https://doi.org/10.1200/jco.2000.18.4.743.
Mardanian-Dehkordi L, Kahangi L. The Relationship between Perception of Social Support and Fatigue in Patients with Cancer. Iran J Nurs Midwifery Res. 2018;23(4):261–6. https://doi.org/10.4103/ijnmr.IJNMR_63_17.
Karakoç T, Yurtsever S. Relationship between social support and fatigue in geriatric patients receiving outpatient chemotherapy. Eur J Oncol Nurs Soc. 2010;14(1):61–7. https://doi.org/10.1016/j.ejon.2009.07.001.
Yellen SB, Cella DF, Webster K, Blendowski C, Kaplan E. Measuring fatigue and other anemia-related symptoms with the Functional Assessment of Cancer Therapy (FACT) measurement system. J Pain Symptom Manage. 1997;13(2):63–74. https://doi.org/10.1016/s0885-3924(96)00274-6.
Van Belle S, Paridaens R, Evers G, Kerger J, Bron D, Foubert J, et al. Comparison of proposed diagnostic criteria with FACT-F and VAS for cancer-related fatigue: proposal for use as a screening tool. Support Care Cancer. 2005;13(4):246–54. https://doi.org/10.1007/s00520-004-0734-y.
Cella D, Peterman A, Passik S, Jacobsen P, Breitbart W. Progress toward guidelines for the management of fatigue. Oncology (Williston Park). 1998;12(11A):369–77.
Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol. 1993;11(3):570–9. https://doi.org/10.1200/jco.1993.11.3.570.
Radloff LS. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Appl Psychol Meas. 1977;1(3):385–401. https://doi.org/10.1177/014662167700100306.
Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23(2):129–38.
Cutrona CE, Russel D. The provisions of social relationships and adaptation to stress. In: WH J, D P, editors. Adv. Pers. Relationships. Greenwich: JAI Press; 1987. p. 37–67.
Godin G, Shephard RJ. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci. 1985;10(3):141–6.
Beaver WL, Wasserman K, Whipp BJ. A new method for detecting anaerobic threshold by gas exchange. J Appl Physiol (Bethesda, Md: 1985). 1986;60(6):2020–7. https://doi.org/10.1152/jappl.1986.60.6.2020.
Whipp BJ, Davis JA, Wasserman K. Ventilatory control of the “isocapnic buffering” region in rapidly-incremental exercise. Respir Physiol. 1989;76(3):357–67. https://doi.org/10.1016/0034-5687(89)90076-5.
Doyle-Baker D, Temesi J, Medysky ME, Holash RJ, Millet GY. An Innovative Ergometer to Measure Neuromuscular Fatigue Immediately after Cycling. Med Sci Sports Exerc. 2018;50(2):375–87. https://doi.org/10.1249/mss.0000000000001427.
Merton PA. Voluntary strength and fatigue. J Physiol. 1954;123(3):553–64. https://doi.org/10.1113/jphysiol.1954.sp005070.
Team RDC. R: A language and environment for statistical computing. R Foundation for Statistical Computing. Vienna2011
Kowarik A, Templ M. Imputation with the R Package VIM. J Stat Softw. 2016;74(7):1–16.
Tibshirani R. Regression Shrinkage and Selection via the Lasso. J Roy Stat Soc: Ser B (Methodol). 1996;58(1):267–88.
Friedman J, Hastle T, Tibshirani R. Regularization Paths for Generalized Linear Models via Coordinate Descent. J Stat Softw. 2010;33(1):1–22.
Benjamini Y, Hochberg Y. On the Adaptive Control of the False Discovery Rate in Multiple Testing With Independent Statistics. J Educ Behav Stat. 2000;25(1):60–83. https://doi.org/10.3102/10769986025001060.
Cohen J. CHAPTER 1 - The Concepts of Power Analysis. In: Cohen J, editor. Statistical Power Analysis for the Behavioral Sciences. Academic Press; 1977. p. 1–17.
Place N, Millet GY. Quantification of Neuromuscular Fatigue: What Do We Do Wrong and Why? Sports Med (Auckland, NZ). 2020;50(3):439–47. https://doi.org/10.1007/s40279-019-01203-9.
Taul-Madsen L, Dalgas U, Kjølhede T, Hvid LG, Petersen T, Riemenschneider M. A Head-to-Head Comparison of an Isometric and a Concentric Fatigability Protocol and the Association With Fatigue and Walking in Persons With Multiple Sclerosis. Neurorehabil Neural Repair. 2020;34(6):523–32. https://doi.org/10.1177/1545968320920250.
Lavigne C, Lau H, Francis G, Culos-Reed SN, Millet GY, Twomey R. Neuromuscular function and fatigability in people diagnosed with head and neck cancer before versus after treatment. Eur J Appl Physiol. 2020;120(6):1289–304. https://doi.org/10.1007/s00421-020-04362-0.
Berger AM. Patterns of fatigue and activity and rest during adjuvant breast cancer chemotherapy. Oncol Nurs Forum. 1998;25(1):51–62.
Winters-Stone KM, Bennett JA, Nail L, Schwartz A. Strength, physical activity, and age predict fatigue in older breast cancer survivors. Oncol Nurs Forum. 2008;35(5):815–21. https://doi.org/10.1188/08.onf.815-821.
Marcora SM, Bosio A, de Morree HM. Locomotor muscle fatigue increases cardiorespiratory responses and reduces performance during intense cycling exercise independently from metabolic stress. Am J Physiol Regul Integr Comp Physiol. 2008;294(3):R874–83. https://doi.org/10.1152/ajpregu.00678.2007.
Myers J, Kaminsky LA, Lima R, Christle JW, Ashley E, Arena R. A Reference Equation for Normal Standards for VO2 Max: Analysis from the Fitness Registry and the Importance of Exercise National Database (FRIEND Registry). Prog Cardiovasc Dis. 2017;60(1):21–9. https://doi.org/10.1016/j.pcad.2017.03.002.
Mitchell SA, Hoffman AJ, Clark JC, DeGennaro RM, Poirier P, Robinson CB, et al. Putting evidence into practice: an update of evidence-based interventions for cancer-related fatigue during and following treatment. Clin J Oncol Nurs. 2014;18(Suppl):38–58. https://doi.org/10.1188/14.cjon.s3.38-58.
Campbell KL, Winters-Stone KM, Wiskemann J, May AM, Schwartz AL, Courneya KS, et al. Exercise Guidelines for Cancer Survivors: Consensus Statement from International Multidisciplinary Roundtable. Med Sci Sports Exerc. 2019;51(11):2375–90. https://doi.org/10.1249/mss.0000000000002116.
Doyle C, Kushi LH, Byers T, Courneya KS, Demark-Wahnefried W, Grant B, et al. Nutrition and physical activity during and after cancer treatment: an American Cancer Society guide for informed choices. CA Cancer J Clin. 2006;56(6):323–53. https://doi.org/10.3322/canjclin.56.6.323.
Ottenbacher A, Yu M, Moser RP, Phillips SM, Alfano C, Perna FM. Population Estimates of Meeting Strength Training and Aerobic Guidelines, by Gender and Cancer Survivorship Status: Findings From the Health Information National Trends Survey (HINTS). J Phys Act Health. 2015;12(5):675–9. https://doi.org/10.1123/jpah.2014-0003.
Courneya KS, Katzmarzyk PT, Bacon E. Physical activity and obesity in Canadian cancer survivors: population-based estimates from the 2005 Canadian Community Health Survey. Cancer. 2008;112(11):2475–82. https://doi.org/10.1002/cncr.23455.
Bellizzi KM, Rowland JH, Jeffery DD, McNeel T. Health behaviors of cancer survivors: examining opportunities for cancer control intervention. J Clin Oncol. 2005;23(34):8884–93. https://doi.org/10.1200/jco.2005.02.2343.
Bower JE. Cancer-related fatigue–mechanisms, risk factors, and treatments. Nat Rev Clin Oncol. 2014;11(10):597–609. https://doi.org/10.1038/nrclinonc.2014.127.
Dantzer R, O’Connor JC, Freund GG, Johnson RW, Kelley KW. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci. 2008;9(1):46–56. https://doi.org/10.1038/nrn2297.
Larson SJ, Dunn AJ. Behavioral effects of cytokines. Brain Behav Immun. 2001;15(4):371–87. https://doi.org/10.1006/brbi.2001.0643.
Trudel-Fitzgerald C, Savard J, Ivers H. Which symptoms come first? Exploration of temporal relationships between cancer-related symptoms over an 18-month period. Ann Behav Med. 2013;45(3):329–37. https://doi.org/10.1007/s12160-012-9459-1.
Ho SY, Rohan KJ, Parent J, Tager FA, McKinley PS. A longitudinal study of depression, fatigue, and sleep disturbances as a symptom cluster in women with breast cancer. J Pain Symptom Manage. 2015;49(4):707–15. https://doi.org/10.1016/j.jpainsymman.2014.09.009.
Ryan JL, Carroll JK, Ryan EP, Mustian KM, Fiscella K, Morrow GR. Mechanisms of cancer-related fatigue. Oncologist. 2007;12(Suppl 1):22–34. https://doi.org/10.1634/theoncologist.12-S1-22.
Visser MR, Smets EM. Fatigue, depression and quality of life in cancer patients: how are they related? Support Care Cancer. 1998;6(2):101–8. https://doi.org/10.1007/s005200050142.
Morrow GR, Hickok JT, Roscoe JA, Raubertas RF, Andrews PL, Flynn PJ, et al. Differential effects of paroxetine on fatigue and depression: a randomized, double-blind trial from the University of Rochester Cancer Center Community Clinical Oncology Program. J Clin Oncol. 2003;21(24):4635–41. https://doi.org/10.1200/jco.2003.04.070.
Tibubos AN, Ernst M, Brähler E, Fischbeck S, Hinz A, Blettner M, et al. Fatigue in survivors of malignant melanoma and its determinants: a register-based cohort study. Support Care Cancer. 2019;27(8):2809–18. https://doi.org/10.1007/s00520-018-4587-1.
Goedendorp MM, Gielissen MF, Verhagen CA, Peters ME, Bleijenberg G. Severe fatigue and related factors in cancer patients before the initiation of treatment. Br J Cancer. 2008;99(9):1408–14. https://doi.org/10.1038/sj.bjc.6604739.
Bower JE, Ganz PA, Dickerson SS, Petersen L, Aziz N, Fahey JL. Diurnal cortisol rhythm and fatigue in breast cancer survivors. Psychoneuroendocrinology. 2005;30(1):92–100. https://doi.org/10.1016/j.psyneuen.2004.06.003.
Fagundes CP, Murray DM, Hwang BS, Gouin JP, Thayer JF, Sollers JJ 3rd, et al. Sympathetic and parasympathetic activity in cancer-related fatigue: more evidence for a physiological substrate in cancer survivors. Psychoneuroendocrinology. 2011;36(8):1137–47. https://doi.org/10.1016/j.psyneuen.2011.02.005.
Charalambous A, Berger AM, Matthews E, Balachandran DD, Papastavrou E, Palesh O. Cancer-related fatigue and sleep deficiency in cancer care continuum: concepts, assessment, clusters, and management. Support Care Cancer. 2019;27(7):2747–53. https://doi.org/10.1007/s00520-019-04746-9.
Fiorentino L, Rissling M, Liu L, Ancoli-Israel S. The Symptom Cluster of Sleep, Fatigue and Depressive Symptoms in Breast Cancer Patients: Severity of the Problem and Treatment Options. Drug Discov Today Dis Model. 2011;8(4):167–73. https://doi.org/10.1016/j.ddmod.2011.05.001.
Acknowledgements
The authors would like to thank the Canadian Cancer Society for funding the study (grant #704208-1). The authors would also like to acknowledge and sincerely thank Dr. Renata Krüger for her assistance with phlebotomy and the careful storage of blood samples, and Doug Doyle-Baker for his assistance with data collection. Finally, the authors would like to thank the participants—without them, this research would not be possible.
Funding
The study was funded by the Canadian Cancer Society (grant #704208–1).
Author information
Authors and Affiliations
Contributions
G.Y.M conceived and designed the study; R.T, J.T, T.M and M.M performed experiments; C.G.B, R.T, J.T and J.G.W analysed data; C.G.B, G.Y.M, R.T interpreted results of experiment; C.G.B drafted manuscript; R.T, J.T, J.G.W, T.M, M.M, N.C.R and G.Y.M edited and revised manuscript. C.G.B, R.T, J.T, J.G.W, T.M, M.M, N.C.R and G.Y.M approved final version of manuscript.
Corresponding author
Ethics declarations
Ethics approval
Approval for all procedures was obtained by the Conjoint Health Research Ethics Board and the Health Research Ethics Board of Alberta Cancer Committee (REB14-0398 and HREBA.CC-16–10-10, respectively). The study was conducted in accordance with all aspects of the Declaration of Helsinki, apart from registration in a database.
Consent to participate
All participants provided written informed consent to take part in the study.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Brownstein, C.G., Twomey, R., Temesi, J. et al. Physiological and psychosocial correlates of cancer-related fatigue. J Cancer Surviv 16, 1339–1354 (2022). https://doi.org/10.1007/s11764-021-01115-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-021-01115-6