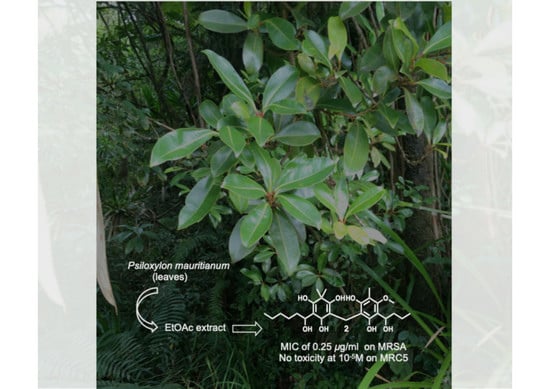
Potent and Non-Cytotoxic Antibacterial Compounds Against Methicillin-Resistant Staphylococcus aureus Isolated from Psiloxylon mauritianum, A Medicinal Plant from Reunion Island
Abstract
:1. Introduction
2. Results and Discussion
3. Materials and Methods
3.1. General Experimental Procedures
3.2. Plant Material
3.3. Extraction and Isolation
3.4. Determination of Minimal Inhibitory Concentration
3.5. Cytotoxicity Evaluation
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ridenour, G.A.; Wong, E.S.; Call, M.A.; Climo, M.W. Duration of colonization with methicillin-resistant Staphylococcus aureus among patients in the intensive care unit: Implications for intervention. Infect. Control Hosp. Epidemiol. 2006, 27, 271–278. [Google Scholar] [CrossRef]
- Schito, G.C. The importance of the development of antibiotic resistance in Staphylococcus aureus. Clin. Microbiol. Infect. 2006, 12, 3–8. [Google Scholar] [CrossRef] [Green Version]
- Chambers, H.F.; DeLeo, F.R. Waves of resistance: Staphylococcus aureus in the antibiotic era. Nat. Rev. Microbiol. 2009, 7, 629–641. [Google Scholar] [CrossRef]
- WHO: World Health Organization. Available online: https://www.who.int/en/news-room/detail/27-02-2017-who-publishes-list-of-bacteria-for-which-new-antibiotics-are-urgently-needed (accessed on 1 June 2020).
- Gibbons, S. Anti-staphylococcal plant natural products. Nat. Prod. Rep. 2004, 21, 263–277. [Google Scholar] [CrossRef]
- Wilson, P.G.; O’Brien, M.M.; Heslewood, M.M.; Quinn, C.J. Relationships within Myrtaceae sensu lato based on a matK phylogeny. Plant Syst. Evol. 2005, 251, 3–19. [Google Scholar] [CrossRef]
- Lavergne, R. Tisaneurs et Plantes Médicinales Indigenes de L’Ile de la Reunion, 3rd ed.; Orphie: Livry Gargan, France, 1990; pp. 160–161. [Google Scholar]
- Mahomoodally, F.M.; Korumtollee, H.N.K.; Khan Chady, Z.Z.B. Psiloxylon mauritianum (Bouton ex Hook.f.) Baillon (Myrtaceae): A promising traditional medicinal plant from the Mascarene Islands. J. Intercult. Ethnopharmacol. 2014, 3, 192–195. [Google Scholar] [CrossRef]
- Clain, E.; Haddad, J.G.; Koishi, A.C.; Sinigaglia, L.; Rachidi, W.; Desprès, P.; Duarte dos Santos, C.N.; Guiraud, P.; Jouvenet, N.; El Kalamouni, C. The Polyphenol-Rich Extract from Psiloxylon mauritianum, an Endemic Medicinal Plant from Reunion Island, Inhibits the Early Stages of Dengue and Zika Virus Infection. Int. J. Mol. Sci. 2019, 20, 1860. [Google Scholar] [CrossRef] [Green Version]
- Rangasamy, O.; Mahomoodally, F.M.; Gurib-Fakim, A.; Quetin-Leclercq, J. Two anti-staphylococcal triterpenoid acids isolated from Psiloxylon mauritianum (Bouton ex Hook.f.) Baillon, an endemic traditional medicinal plant of Mauritius. S. Afr. J. Bot. 2014, 93, 198–203. [Google Scholar] [CrossRef] [Green Version]
- Chen, N.-H.; Zhang, Y.-B.; Huang, X.-J.; Jiang, L.; Jiang, S.-Q.; Li, G.Q.; Yao-Lan Li, Y.-L.; Wang, G.-C. Drychampones A−C: Three Meroterpenoids from Dryopteris championii. J. Org. Chem. 2016, 81, 9443–9448. [Google Scholar] [CrossRef]
- Ito, H.; Muranaka, T.; Mori, K.; Jin, Z.-X.; Tokuda, H.; Nishino, H.; Yoshida, T. Ichthyotoxic Phloroglucinol Derivatives from Dryopteris fragrans and Their Anti-tumor Promoting Activity. Chem. Pharm. Bull. 2000, 48, 1190–1195. [Google Scholar] [CrossRef] [Green Version]
- Dais, P.; Plessel, R.; Williamson, K.; Hatzakis, E. Complete 1H and 13C NMR assignment and 31P NMR determination of pentacyclic triterpenic acids. Anal. Methods 2017, 9, 949–957. [Google Scholar] [CrossRef]
- Socolsky, C.; Hernández, M.A.; Bardón, A. Studies in Natural Products Chemistry, 1st ed.; Elsevier: Amsterdam, The Netherlands, 2012; Chapter 5; pp. 105–157. [Google Scholar]
- Widén, C.-J.; Lounasmaa, M.; Sarvela, J. Phloroglucinol Derivatives of eleven Dryopteris species from Japan. Planta Med. 1975, 28, 144–164. [Google Scholar] [CrossRef]
- Li, N.; Gao, C.; Peng, X.; Wang, W.; Luo, M.; Fu, Y.J.; Zu, Y.G. Aspidin BB, a phloroglucinol derivative, exerts its antibacterial activity against Staphylococcus aureus by inducing the generation of reactive oxygen species. Res. Microbiol. 2014, 165, 263–272. [Google Scholar] [CrossRef]
- Gao, C.; Guo, N.; Li, N.; Peng, X.; Wang, P.; Wang, W.; Luo, M.; Fu, Y.-J. Investigation of antibacterial activity of aspidin BB against Propionibacterium acnes. Arch. Dermatol. Res. 2016, 308, 79–86. [Google Scholar] [CrossRef]
- Kabsch, W. XDS. Acta Cryst. 2010, D66, 125–132. [Google Scholar] [CrossRef] [Green Version]
- Evans, P.R.; Murshudov, G.N. How good are my data and what is the resolution? Acta Cryst. 2013, D69, 1204–1214. [Google Scholar] [CrossRef]
- Vonrhein, C.; Flensburg, C.; Keller, P.; Sharff, A.; Smart, O.; Paciorek, W.; Womack, T.; Bricogne, G. Data processing and analysis with the autoPROC toolbox. Acta Crystallogr. D 2011, 67, 293–302. [Google Scholar] [CrossRef] [Green Version]
- Sheldrick, G.M. SHELXT- Integrated space-group and crystal-structure determination. Acta Crystalogr. A 2015, 71, 3–8. [Google Scholar]
- Sheldrick, G.M. Crystal structure refinement with SHELXL. Acta Crystallogr. C 2015, 71, 3–8. [Google Scholar] [CrossRef]
- European Committee on Antimicrobial Susceptibility Testing EUCAST. Available online: http://www.eucast.org (accessed on 11 April 2016).
- Sorres, J.; Sabri, A.; Brel, O.; Stien, D.; Eparvier, V. Ilicicolinic acids and ilicicolinal derivatives from the fungus Neonectria discophora SNB-CN63 isolated from the nest of the termite Nasutitermes corniger found in French Guiana show antimicrobial activity. Phytochemistry 2018, 151, 69–77. [Google Scholar] [CrossRef]
- EUCAST Definitive Document EDef 7.1: Method for the determination of broth dilution MICs of antifungal agents for fermentative yeasts. Clin. Microbiol. Infect. 2008, 15, 398–405.
- EUCAST Discussion Document, E.Dis 5.1: Determination of minimum inhibitory concentrations (MICs) of antibacterial agents by broth dilution. Clin. Microbiol. Infect. 2003, 9, 1–7.
Sample Availability: Samples of the compounds are available from the authors. |


| Position | Aspidin VB | ||||
|---|---|---|---|---|---|
| δC1 | δH(J in Hz) 2 | COSY | HMBC | ROESY | |
| 1 | 111.9 | ||||
| 2 | 188.4 | ||||
| 3 | 108.9 | ||||
| 4 | 199.9 | ||||
| 5 | 45.1 | ||||
| 6 | 172.7 | ||||
| 7 | 17.7 | 3.57, s | C1, C2, C6, C1′, C2′, C6′ | ||
| 8 | 207.5 | ||||
| 9 | 41.6 | 3.19, dd (7.2, 7.2) | H8 | C3, C8, C10, C11 | H11 |
| 10 | 25.3 | 1.67, m | H9, H11 | C8, C9, C11, C12 | |
| 11 | 32.5 | 1.39, m | H10, H12 | C12 | H9 |
| 12 | 23.2 | 1.38, m | H11, H13 | C11 | |
| 13 | 14.3 | 0.93, t (7.1) | H12 | C11, C12 | |
| 1′ | 110.2 | ||||
| 2′ | 160.6 | ||||
| 3′ | 108.5 | ||||
| 4′ | 161.5 | ||||
| 5′ | 113.2 | ||||
| 6′ | 163.6 | ||||
| 7′ | 62.1 | 3.80, s | C4′ | H9′ | |
| 8′ | 208.0 | ||||
| 9′ | 44.8 | 3.15, dd (7.2, 7.2) | H10′ | C8′, C10′, C11′ | H7′ |
| 10′ | 18.8 | 1.72, sex (7.4) | H9′, H11′ | C8′, C10′, C11′ | |
| 11′ | 14.2 | 0.98, t (7.4) | H10′ | C9′, C10′ | H9′ |
| 12′ | 9.5 | 2.10, s | C4′, C5′, C6′ | H7′ | |
| 6-OH | 10.05, s | C1, C5, C6 | H7, 2′-OH, 6′-OH | ||
| 2′-OH | 15.86, s | C1′, C3′, C8′ | 6-OH | ||
| 6′-OH | 11.41, s | C1′, C5′, C6′ | H7, 6-OH | ||
| Compounds | MIC (µg/mL) | MRC5 Cell Viability (%) | ||||
|---|---|---|---|---|---|---|
| C. albicans ATCC 10213 | T. rubrum SNB-TR1 | S. aureus ATCC 29213 | MRSA ATCC 33591 | 10−5 M | 10−6 M | |
| 1 | >256 | >256 | 2 | 1 | 86 ± 3 | 104 ± 1 |
| 2 | >256 | 256 | 0.25 | 0.25 | 99 ± 2 | 105 ± 2 |
| Crude extract | 8 | 256 | 8 | nd | 96 ± 2 | 100 ± 3 |
| Fluconazole 1 | 1 | 4 | nd | nd | nd | nd |
| Itraconazole 1 | <0.5 | <0.5 | nd | nd | nd | nd |
| Oxacillin 1 | nd 2 | nd | 0.25 | nd | nd | nd |
| Vancomycin 1 | nd | nd | nd | 4 | nd | nd |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sorres, J.; André, A.; Elslande, E.V.; Stien, D.; Eparvier, V. Potent and Non-Cytotoxic Antibacterial Compounds Against Methicillin-Resistant Staphylococcus aureus Isolated from Psiloxylon mauritianum, A Medicinal Plant from Reunion Island. Molecules 2020, 25, 3565. https://doi.org/10.3390/molecules25163565
Sorres J, André A, Elslande EV, Stien D, Eparvier V. Potent and Non-Cytotoxic Antibacterial Compounds Against Methicillin-Resistant Staphylococcus aureus Isolated from Psiloxylon mauritianum, A Medicinal Plant from Reunion Island. Molecules. 2020; 25(16):3565. https://doi.org/10.3390/molecules25163565
Chicago/Turabian StyleSorres, Jonathan, Amandine André, Elsa Van Elslande, Didier Stien, and Véronique Eparvier. 2020. "Potent and Non-Cytotoxic Antibacterial Compounds Against Methicillin-Resistant Staphylococcus aureus Isolated from Psiloxylon mauritianum, A Medicinal Plant from Reunion Island" Molecules 25, no. 16: 3565. https://doi.org/10.3390/molecules25163565